The UPMC Center for Balance Disorders utilizes a multidisciplinary approach, as a balance disorder may be a sign of other medical problems. Collaborating with otolaryngology, physical therapy, neurology, and audiology helps guarantee a comprehensive approach to diagnosis and treatment, beginning with determining the cause. The Center has state-of-the-art technology and a specialized Vestibular Laboratory, which offers several tests to evaluate balance.
 | Joseph M. Furman, MD, PhD, FAAN
|
Dr. Furman’s research interests at the present time concern improving diagnostic testing of the human inner ear balance (vestibular) system. The vestibular system of the inner ear consists of a group of five sensors on each side of the head, so 10 sensors in all. Six of the sensors respond to rotation, i.e., turning, of the head and four of the sensors respond to tilting the head. At this time, even the most advanced testing facilities can only reliably test two of the six rotational sensors. The other four rotational sensors, a full 40% of the vestibular system, cannot be tested. Dr. Furman is developing a recently patented technology for testing these four sensors in a balance laboratory.

Dr. Furman is also developing a less expensive technology that can be easily transported and used in the clinic. Both of these technologies rely on high resolution, high speed, infrared cameras to record eye movements while highly accurate gyroscopes and inclinometers measure movement of the head. A computer then processes this information to provide an assessment of the four sensors of the vestibular system that are not currently being evaluated. This research is being performed in collaboration with a local technology company and has been funded by a combination of the National Institutes of Health and the Department of Defense.
 | Susan L. Whitney, DPT, PhD, NCS, ATC, FAPTA
|
Dr. Whitney is currently funded by two Department of Defense (DoD) grants that support warfighter recovery from mild brain injury with resultant dizziness and balance dysfunction. The PRAXIS study is a multisensory complex retraining program using virtual reality, Stroop tasks, and complex spatial navigation tasks in rehabilitation at the San Antonio Center for the Intrepid.

At the University of Pittsburgh, we are working on a different DoD grant to determine if an app on a tablet can enhance recovery after a vestibular disorder. The app utilizes facial and eye recognition software to record exercise performance with the goal of providing feedback to the patient and physical therapist to optimize the exercise prescription and get people better faster. With colleagues in New Zealand, Dr. Whitney is working with a team to determine the influence of tinnitus on outcomes after mild brain injury and recently completed a large randomized clinical trial with Drs. Sparto, Kontos and others about the effect of exercise dosing on recovery.
In the clinic we are prospectively collecting data about benign paroxysmal positional vertigo (BPPV) by recording precise eye movements. The goal is to try to recognize patterns of eye movements and then determine which canalith repositioning maneuver is most effective for specific eye patterns of nystagmus. Dr. Whitney is actively engaged in studies with others related to persons with BPPV including recognizing new forms of BPPV, BPPV in older persons related to falls, and comments to the World Falls guidelines related to BPPV.
 |
|
Dr. Dunlap's research combines clinical and health services methods to explore factors that influence recovery and patient outcomes in people with balance and vestibular disorders. A primary focus of her work is understanding how fear of movement and activity avoidance affect recovery after a vestibular diagnosis. Dr. Dunlap's research also examines healthcare quality among individuals with vestibular disorders, aiming to identify and address gaps in care. By addressing individual and healthcare-related barriers, Dr. Dunlap’s long-term goal is to enhance quality of care, promote the adoption of evidence-based practices, and improve quality of life and safe mobility for those experiencing dizziness.
 |
|
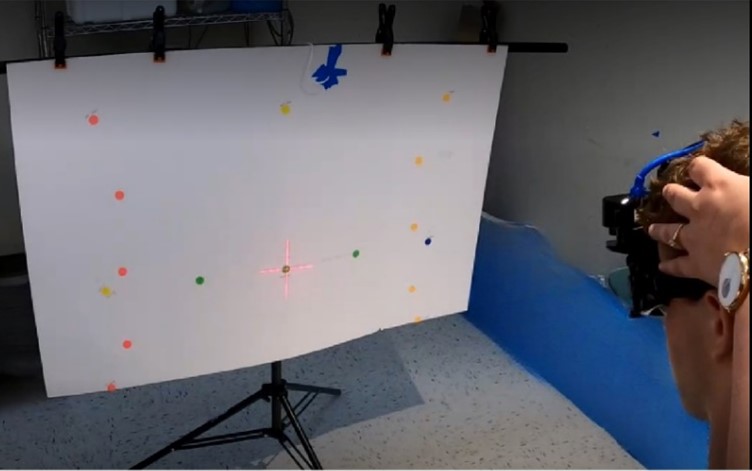
Dr. Harrell is developing a new video head impulse test (vHIT) aimed at enhancing the precision and reliability of diagnosing dizziness, especially in patients with vestibular hypofunction. This innovative diagnostic tool seeks to better identify specific impairments, which could, in turn, inform more targeted rehabilitation interventions to enhance patients’ functional outcomes and overall quality of life.
In addition to her work on vHIT, Dr. Harrell is also deeply invested in understanding the relationship between benign paroxysmal positional vertigo (BPPV) and traumatic brain injury (TBI). She has published several research articles examining how these two conditions interact and the significant functional challenges faced by individuals who experience both BPPV and TBI. Her research aims to inform clinical practice by shedding light on the functional implications and potential rehabilitation strategies for managing these co-occurring diagnoses, ultimately contributing to more holistic and effective care for those with complex vestibular and neurologic conditions.
 |
|
During her post-doctoral fellowship, Dr. Klatt investigated the interplay between vestibular and cognitive function. She continues to investigate this line of research, and in addition to cognition, is interested in exploring other factors that are associated with activity and participation in people with vestibular disorders. Dr. Klatt is currently funded by the National Institutes of Health to conduct her research aiming to optimize vestibular rehabilitation delivery and outcomes.
